5 Questions Doctors Wish Every Patient Would Ask
When is the last time you had a great conversation with your doctor—one where you felt like an active participant in your care?
For many of us, we show up to our healthcare visits as good listeners, assuming our clinicians will take charge and manage our care for us. But in an ideal world, we’d all take more of a leadership role when it comes to our health, says primary care doctor Lucy McBride, MD, author of the popular newsletter Are You Okay? and the forthcoming book, The Empowered Patient: A Doctor's Guide to Reclaiming Your Health. “Unfortunately, our medical system makes us believe that we’re just passive recipients of blood tests and bad luck,” says Dr. McBride. “But I want people to understand that we have so much more control over our health than we think.”
The best way to take the reins and feel like you have true agency at every healthcare visit? Spark conversations with your doctor that go beyond the basics by asking the right questions and bringing them the kind of information that’ll help them optimally care for you, adds Ezekiel J. Emanuel, MD, PhD, an oncologist, world leader in health policy and bioethics, and author of the forthcoming book, Eat Your Ice Cream: Six Simple Rules for a Long and Healthy Life. “Sometimes, just as important as the questions you ask is the information you give your doctors to help them give you the best advice,” he says.
So, what is that information you should bring to your next appointment and what are the questions you can ask your provider that’ll help you have more productive, proactive visits—ones where you feel in control of your health at every age? Read on.
Question No. 1: What vaccines and screening tests do I need?
It’s helpful to have a basic sense of the key vaccinations and health screenings recommended at every decade so you can make sure you’re talking about which ones you need based on your personal and family health history, says Dr. Emanuel.
First, ask about the HPV vaccine if you didn’t get it as a young person, which is approved for adults under age 45. The shingles vaccine is important to get when you turn 50. “Often people overlook this vaccine—until they get shingles. But why go through the pain?” says Dr. Emanuel. “There’s also increasing evidence that the shingles vaccine reduces the chance of cognitive decline and dementia. It’s like a two-for-one.” Two other important vaccines to get when you hit age 50: the RSV (respiratory syncytial virus) and pneumococcal pneumonia vaccines.
As for health screenings, these are dependent on your personal and family health history. (Good reason to arrive at your doctor’s appointments prepared with as complete a personal and family health history as possible.) Talk to your clinician about an annual full-body skin cancer screening, mammogram (which is recommended starting at age 40 for most) and a colonoscopy (which start at age 45, unless there’s a reason to do it sooner). And if you’re a smoker or former smoker, talk to your doctor about when to begin lung cancer screening.
Dr. Rocio Salas-Whalen, a leading weight management expert and board-certified specialist in obesity medicine and endocrinology and author of the forthcoming book, Weightless: A Doctor’s Guide to GLP-1 Medications, Sustainable Weight Loss, and the Health You Deserve, recommends asking for a body composition exam—especially if you’ve been saying, “I need to lose 10 pounds” a few years in a row. This exam measures the proportion of fat, bone, and muscle in your body, which gives you a much better picture of health than weight alone and can give you a good picture of your starting point if you’re about to make some changes to your diet and exercise routine.
For a healthy woman, percentage of body fat should be between 18 and 28 percent, says Dr. Salas-Whalen. And visceral fat—the “bad” fat that surrounds your internal organs and is pro-inflammatory—should be as low as possible. You also want skeletal muscle (that’s the muscle you can work and grow) to hover around 30 percent or more.
Question No. 2: This is my typical diet and exercise routine. How does it sound to you?
Dr. Emanuel recommends starting with specifics about your diet—especially if you’re vegan, vegetarian, or pescatarian, as these diet variations have implications when it comes to making sure you’re getting enough important nutrients. For example, vegans and vegetarians are often low on vitamin B12 and may need a supplement. If you eat meat, you might share how frequently you eat fish (and what types) to give your clinician a sense of whether or not you’re getting enough important omega-3 fatty acids from your diet alone.
Also, it’s important to be honest about how much you’re snacking. “This is one of the most shocking trends in America that doesn’t get enough attention,” says Dr. Emanuel. “We’re eating 500 more calories per day—for those keeping score, that’s a pound a week—of snack foods like muffins, cakes, cookies, and pretzels.” Talking through this with your doctor can help you talk through healthier options you might reach for when a snack attack hits, like fruit, nuts, yogurt, or another balanced nosh.
In addition to bringing up specifics about your diet, you’ll want to do the same for your exercise routine. How many days a week do you work out, and what do you do? And yes, your doctor will be listening intently to see if you’re doing the one type of exercise that we’re collectively talking a lot more about these days: strength training.
“As we get older, our lean muscle goes down—and it goes down pretty substantially, especially after around age 60,” says Dr. Emanuel. “Maintaining this muscle mass by resistance training and eating enough protein gets more important as we age, not less important.”
If you’re in your 20s and 30s, now is the time to bank as much muscle as you can. Bonus: This is when it’s easiest to build and maintain, says Dr. Salas-Whalen. Once you hit your 40s and beyond, you have to work harder to gain and maintain muscle—but it’s an effort that really does pay off. “That’s because muscle is our super organ,” says Dr. Salas-Whalen. “Muscle produces a hormone called myokine, which is anti-inflammatory. Every time a muscle contracts, it absorbs glucose from the bloodstream, which improves insulin sensitivity. And building muscle improves your body’s support structure, helping you age independently into your 70s, 80s, 90s, and beyond.”
The bottom line: It’s never too late to start strength training, and it really does work when it comes to improving multiple health outcomes.
Question No. 3: What’s the highest yield thing I can do for my health when it comes to my nutrition, exercise, and mental health?
Dr. Lucy McBride, MD, understands that most of us can’t be (or don’t want to be) Peter Attia disciples who cold-water plunge and organize our lives around grams of protein. But she does want each of us to ask, “What are the highest yield things I can do to help my health? And how can I operationalize these things in my life?” In other words, what’s going to give you the biggest health bang for your proverbial buck that actually feels doable?
For example, maybe it means getting genetic testing for breast cancer given your family history, or it’s finally seeing a pelvic floor specialist to fix that hip asymmetry or urinary incontinence you’re still dealing with after three pregnancies. Maybe what would really move the needle for you is aiming to get just an hour more sleep each night or quitting alcohol. “Stop focusing on the supplements and the optimization,” says Dr. McBride. “Oftentimes the most important medical interventions are the simplest.” Talk to your doctor about what those might be for you.
Question No. 4: Am I a candidate for a GLP-1 medication? (Or, if you’re taking one, the essential question to ask is: Am I doing everything I can to counter the muscle loss that often comes with fat loss when taking this medication?)
In recent years, there’s been a major increase in the number of Americans taking GLP-1 drugs for weight loss. Nearly 12 percent of Americans have taken these medications, including about one-fifth of women between 50 and 64, according to a RAND report. Dr. Salas-Whalen, a leading weight management expert and specialist in obesity medicine and endocrinology, believes even more patients should be having a conversation with their doctors about whether they are a candidate.
“Too many people see GLP-1s as ‘the easy way out’ or ‘cheating,’” says Dr. Salas-Whalen. “What I want more people to know is that a GLP-1 should not be the last resort. You don’t have to earn the right to be on one of these medications.”
What is crucial, however, is to work with a physician who has expertise prescribing this medication—and one who’ll have a conversation with you about the importance of strength training and increasing your protein intake (to at least 100 grams a day) if you’re taking one of these meds. “If you’re not having this conversation—and tracking muscle maintenance with body composition scans every 10 to 12 weeks—you’re with the wrong doctor,” says Dr. Salas-Whalen.
Question No. 5: Am I being as proactive as I can be now that I’m in menopause (for women) or andropause (for men)?
We’re collectively talking more about the menopause transition and its implications on our health, which is a great thing. It has meant more of us are bringing up this once-taboo topic with our doctors, talking about symptoms we’re experiencing, and understanding treatment options like menopause hormone therapy. This is a great thing. If you’re a woman in midlife, bringing this important hormonal transition up with your doctor can help you make sure you’re doing all that you can to optimize your health trajectory.
For men, this conversation about changing hormones is equally important though much less talked about, says Florence Comite, MD, founder and CEO of Comite Center for Precision Medicine & Healthy Longevity and author of Keep It Up: The Power of Precision Medicine to Conquer Low T and Revitalize Your Life. “Most of the time, men think they’re healthy until they get a heart attack,” she says. “But it’s important for men to know that they go through all the same shifts as women do, just at different rates and in different times.”
That’s right: Men go through their own version of menopause, called andropause—and their own version of perimenopause, called periandropause.
“Testosterone, which men have in much greater amounts than women, drops every year—and this really impacts them,” says Dr. Comite. There’s a whole constellation of symptoms that are similar to women going through menopause, she adds: low energy; a decline in sexual function; weight creep around the middle; even hot flashes and cold flushes. These symptoms aren’t just bummers of aging to brush off. They are important topics to bring up with your healthcare team.
“When your testosterone is low, you have a 30 to 40 percent increased risk of heart disease, stroke, osteoporosis, and other health conditions,” says Dr. Comite. It’s crucial to talk through what you can do to counter some of these age-related hormonal changes. (Hint: It’s a lot of the same advice for both sexes, including strength training to build and maintain muscle, eating a balanced diet that includes adequate protein, limiting or eliminating alcohol, and getting plenty of sleep.)
In the end, these questions aren’t just about optimizing your health and getting better care. They’re about helping you become the CEO of your own healthcare and feeling confident to speak up and keep asking the right questions of your doctors as your body—and life—changes. When you advocate for yourself, you send a powerful message: I’m paying attention. I matter. I’m here to work with you. And that’s a mindset that has the power to transform your health now and for many years to come.
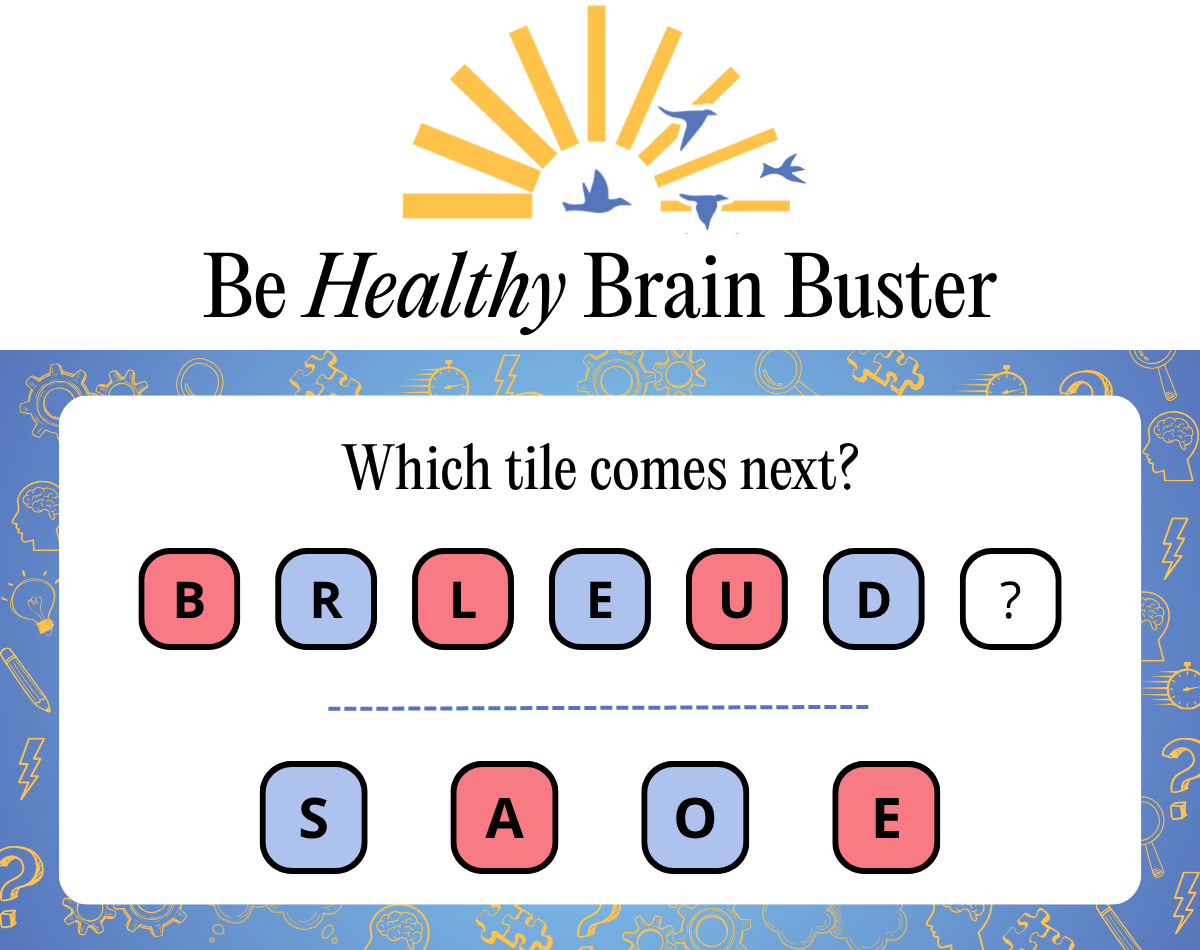
Answer
E. The blue tiles spell RED, and the red tiles spell BLUE, alternating with each other.
Meghan Rabbitt is an editor and writer for The Sunday Paper and author of The New Rules of Women’s Health: Your Guide to Thriving at Every Age, which you can order here.
Please note that we may receive affiliate commissions from the sales of linked products.




