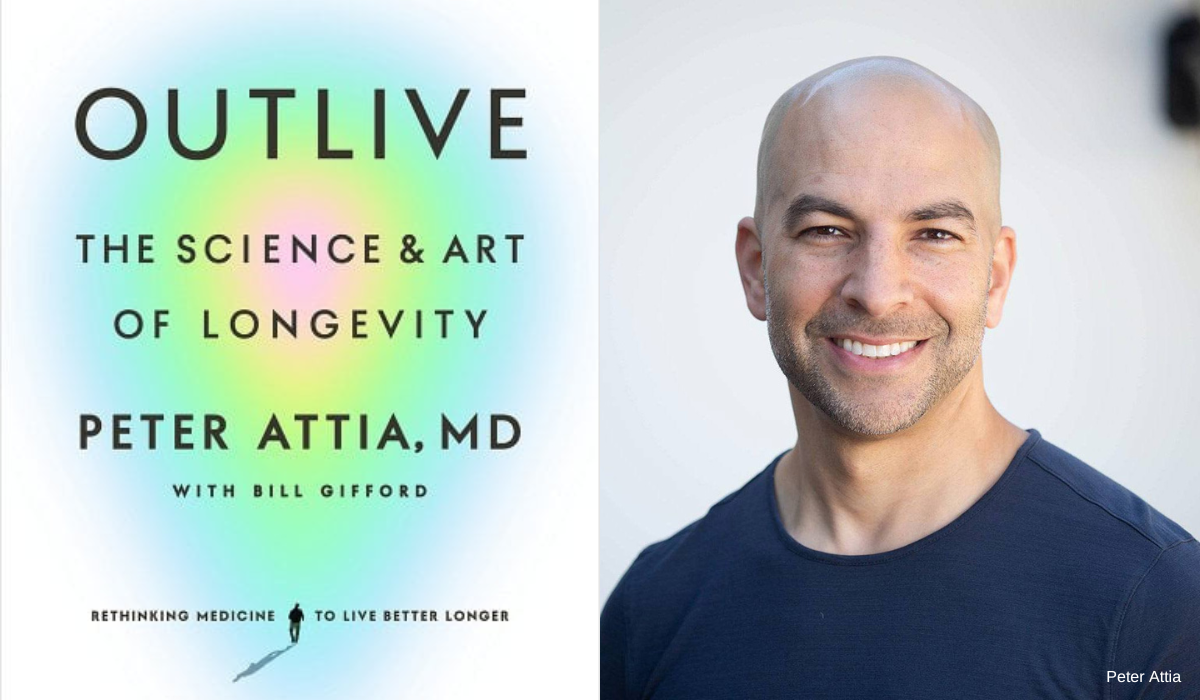
We All Want to Live Better, Longer. Dr. Peter Attia's New Bestselling Book Can Help All of Us Do Just That
Dr. Peter Attia doesn’t particularly like the word “longevity.”
Sure, it’s in the title of his new book, “Outlive: The Science and Art of Longevity.” And yes, he knows that all of us are after it.
It’s just that the former surgeon and wildly popular podcaster says the word too often inspires extreme views. “On one hand, there’s a sort of sci-fi aspect to how people think about longevity—like it’s just a matter of time until we come up with this magic pill and we don’t have to do anything until then because technology will solve all the problems for us,” Dr. Attia told The Sunday Paper.
The word also disproportionately emphasizes lifespan (put simply, the number of years you live) and doesn’t put enough emphasis on healthspan (a more nuanced concept that has to do with preserving three elements of health for as long as possible: cognitive, physical, and emotional), says Dr. Attia. “I think longevity is a reasonable word, but it does require explanation to make sure we understand all that it encompasses,” he adds.
In his new book, Dr. Attia aims to do just that. We sat down with the Austin, Texas-based doctor to talk about what all of us can do to improve both our lifespan and healthspan, starting today.
A CONVERSATION WITH DR. PETER ATTIA
One of your core principles is that the only way to set yourself on a better health trajectory is to start thinking about it and acting now. Where should we start?
I hope the book answers that question for people in a way that’s relative and personal for them. The truth is there isn’t a single answer. If a person’s reading the book, they might come to the conclusion that their sleep is horrible—and if that’s not in order, worrying about the finer details of what you’re eating or how you’re exercising is futile. That person’s sleep needs to be addressed first. What I hope the book does is inspire people to find their low-hanging fruit.
When I started writing this book six years ago, I had one clear intention: In 10 years, I want the book to still be relevant. That’s tough to do. If you write books that are just tactical—do this specific workout, eat this not that—they won’t be relevant for very long. The only way I could write something with enduring value was to write a book that had scaffolding for people to build on. In 10 years, I’ll likely be doing things differently than I’m doing them today; I’ll be prescribing different things to my patients. That’s the progress of science. But the foundation on which that advice is given is largely constant. My main objective with this book was to build something valuable over the long-term.
Throughout the book you talk about Medicine 3.0 and how it’s crucial if we want to live better, longer. What is Medicine 3.0?
To explain it, you have to have some understanding of what Medicine 1.0 and Medicine 2.0 are.
Medicine 1.0 is basically the medicine that dominated our existence up until the middle to later part of the 19th century. It was the medicine that had no foundation of science; we had no idea what we were doing and as a result, we were making stuff up. The gods controlled things. It was very superstitious.
Then some very important technological breakthroughs happened, namely the development of the microscope, and we realized: There’s this microscopic world, and when coupled with sanitation techniques and antibiotics, we heralded in Medicine 2.0. This is the modern era of medicine, which has been very successful at treating what I call fast death—trauma, infections, those sorts of things. However, we are effectively abutting—and have been for some time—the limits of what Medicine 2.0 can do. That’s evidenced by the fact that we saw enormous improvement of human longevity when that transition from Medicine 1.0 to Medicine 2.0 took place. It was approximately a doubling of human lifespan, from age 40 to age 80, that took place in a relatively short period of time.
But when you take that life expectancy of age 80 that we have today and strip out the most common causes of death, our life expectancy is just as bad as it was at the turn of the last century. In other words, we really haven’t done anything to live longer when it comes to preventing slow death. And that’s where Medicine 3.0 comes along.
Medicine 3.0 has to do a few things Medicine 2.0 can’t do. It has to have the tools to prevent chronic disease, or at least delay their onset significantly. That’s a very important distinction. Medicine 2.0 focuses on treating chronic disease—i.e., lengthening the period of time you live with a chronic disease. Medicine 3.0 says, We’ve done that experiment, it’s failed, and oh, by the way, longer life means living longer without disease, not with disease.
Prevention has to be something that is real. It can’t be a lip service token, and the people who administer that prevention—namely physicians—have to understand the nuances of nutrition, exercise, sleep, distress tolerance, just as much as they understand the nuance of prescribing medications.
What’s your advice for finding a “Medicine 3.0” practitioner—someone who takes a similar, proactive approach as you do?
I think there are plenty of doctors out there who take this approach. You have to be as thoughtful about selecting physicians as you are about selecting other professionals in your life. If someone said to you, “Go and hire an architect to build your house,” I don’t think you’d go on Google and search “architect” and use the first person to come up. In hiring a nanny to take care of your kids, you wouldn’t randomly pick a person who happened to have a convenient location. Think about the due diligence you put into other areas of your life, and realize you have to do the same in medicine.
Also, know that if a doctor is going to be practicing Medicine 3.0, they’ll have to have done a lot of learning on their own. Because none of us learned this in medical school or residency; it’s simply not taught.
The last chapter of your book is a powerful—and very personal—look at the importance of emotional health. Why is our emotional wellbeing so closely tied to our lifespan and healthspan?
I think there’s been a lot of emphasis on the relationship between emotional health and lifespan. The most extreme example of this is that people kill themselves. Suicide is in the top 10 causes of death for every demographic above the age of 11. That’s a frightening statistic. But I think that’s really just the tip of the iceberg. If you expand outside the circle of suicide, you get what’s called parasuicide and deaths of despair. If you look at accidental overdoses or accidental poisoning due to Fentanyl, or toxins that are put into illicit drugs, over 100,000 people in the U.S. succumbed to that in the last year, which is actually more than all suicides.
If you expand that even more and look at deaths attributed to alcohol excess—everything from cirrhosis to drinking and driving accidents that result in fatalities—now we’re talking about a couple hundred thousand people a year. Then, let’s go even further than that and not just bracket it by a shortened life, but talk about quality of life and healthspan. It’s a very simple thought experiment: If you were granted eternal life, but you couldn’t share that with anyone, would it be worth it? Nobody would choose that, right? Even if you were granted perfect health, it would be a totally lonely and miserable existence.
So, you start to realize an important fabric of living a good life is having good relationships. And having good relationships with others generally requires having a good relationship with yourself. On my own journey, through coming to understand these things and addressing my own issues, I realized I probably needed to share this on some level. I think it would’ve been disingenuous to write this book as the operating manual for just the physical side of living longer and living better.
We’re living in times when so many of us are sick. A lot of people feel like it’s hard to make a change—both societally and individually. Is there hope?
I can’t speak to the societal level. That’s just something any individual shouldn’t have to worry about. I don’t want to use the challenges of fixing problems in society as an excuse for not fixing problems as an individual. But if you’re an individual reading this thinking, I’ve blown it. I’m 50 years old, I’m obese, I have type 2 diabetes, it’s over, it’s not true. The data will tell you that you can undo that damage.
We know, for example, if you’ve been smoking a pack a day, by the time you’re 50 years old your risk of death is 40% higher in the coming year than a non-smoker. However, once you quit, within about 15 years—so, by the time you’re 65—your risk is almost the same as a person who’s never smoked.
There are countless stories of people who completely turn their lives around, but you have to take that first step. You have to say, OK, tomorrow’s going to be a better day than today, because maybe I’ve never lifted a finger in my life vis a vis direct exercise, but I’m going to go walk for 10 minutes today. And the next day, I’m going to walk for 10 minutes again. After a month of walking 10 minutes every day, you’ll have demonstrated that you have the capacity to exercise. It’s become a part of your routine. And you might say, Maybe I’ll start walking for 20 minutes a day.
When you do this, you’ll start to see that the inconvenience of having to do this new healthy thing is dwarfed by the benefits you’ll start seeing.
Of all the research you’ve put into this book, is there anything that surprised you the most?
There was a lot of data that surprised me, but one that stands out is learning about the severity of hip fractures. When I came across the data for what the one-year mortality was for people over the age of 65 who fell and broke their hips or femurs, I thought it couldn’t be right. Somewhere between 10% to 30% of people who fall and break their hip or femur will be dead within a year. That’s an astonishing fact to wrap your mind around. And by the way, that doesn’t even tell you about the equally devastating corollary to that: Of the people who are not dead after they fracture a hip, they’re often debilitated to the point where their quality of life is never the same. And you could argue they might as well be dead in a different way.
Another surprise was how exercise is such a powerful tool. There’s the lip service answer we all know, which is “Exercise is good for you.” But I don’t think people fully appreciate how powerful it is. Having a high cardiorespiratory fitness, having muscle mass, being strong for your age and sex—these things confer far greater benefit in magnitude than any negative thing confers harm. It’s not close. That means smoking, diabetes, end stage kidney disease, hypertension—those things on the bad side of the ledger are not as large in magnitude as high strength, fitness, and muscle mass are on the positive side of the ledger.
What do you hope readers will take away from this book?
I want people to make a change in their life that sticks in whatever area they most need it. There might be some people for whom reading this book is the ticket they need to start lifting weights. Maybe they’ve been afraid to lift weights. This book hopefully demystifies it a bit and a reader will say, “You know, I’m a 65-year-old woman who’s never touched weights in her life, but Peter’s made a case that I need to hire a trainer and start doing this thing.”
I also hope that if someone finds themselves in the same emotional state I was in six years ago, they’re able to believe that whatever they’re struggling with—whatever character flaws they see in themselves—are not permanent. Those things can be changed just as much as you can change the state of your physical health.
Peter Attia, MD, is the founder of Early Medical, a medical practice that applies the principles of Medicine 3.0 to patients with the goal of lengthening their lifespan and simultaneously improving their healthspan. He is the host of The Drive, one of the most popular podcasts covering the topics of health and medicine. Dr. Attia received his medical degree from the Stanford University School of Medicine and trained for five years at the Johns Hopkins Hospital in general surgery. He lives in Austin, Texas with his wife and three kids.
Question from the Editor: What is the low-hanging fruit in your life—the area in which you can make improvements for your lifespan and healthspan?
Please note that we may receive affiliate commissions from the sales of linked products.